Estrogen, Progesterone, and Breast Pain

Have you ever found yourself wincing at a sudden jolt of breast tenderness? Understanding the connection between hormone fluctuations and breast pain is key to managing this common discomfort effectively. Let’s explore the critical insights that can empower you to take control of your breast health.
What You Will Learn
- The roles of estrogen and progesterone in breast tissue sensitivity and health.
- How to differentiate between cyclic and noncyclic breast pain.
- The importance of tracking hormonal fluctuations for better symptom management.
- Empowering strategies to alleviate breast pain and enhance well-being.
Hormonal Influence on Breast Pain
Understanding the interplay between key hormones and breast pain, categorized into cyclic and noncyclic types.
Estrogen: The Growth Stimulator
Typically peaks in the first half of the menstrual cycle, promoting breast tissue growth and density. This can lead to increased sensitivity.
Progesterone: The Tenderness Inducer
Rises in the second half of the cycle, preparing breasts for potential pregnancy, often leading to swelling and tenderness.
Cyclic Mastalgia: Hormonal Link
Directly related to hormonal fluctuations during the menstrual cycle, peaking before menstruation. Predictable patterns.
Noncyclic Mastalgia: Other Factors
Less predictable and not directly linked to hormonal cycles. Can be influenced by stress, injury, or other underlying conditions.
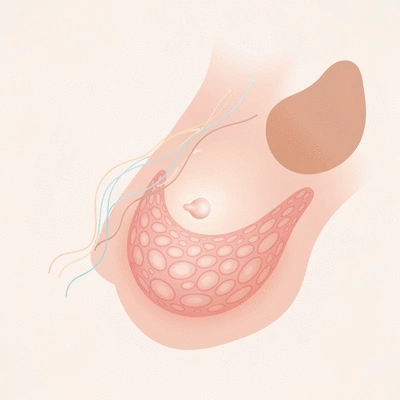
Exploring the Connection Between Hormones and Breast Pain
Have you ever wondered why your breasts feel tender at certain times during the month? The answer often lies in the intricate dance of hormones, particularly estrogen and progesterone. Understanding how these hormones fluctuate during your menstrual cycle can provide significant insights into breast tissue health and tenderness. In this section, we will explore the roles of these hormones and their impact on breast health.
As your menstrual cycle progresses, your body goes through various hormonal changes that directly affect breast tissue. Estrogen levels typically rise in the first half of your cycle, leading to increased sensitivity. This is often followed by a surge in progesterone during the second half, which can compound the feeling of tenderness. By tracking these fluctuations, you can become more attuned to your body’s signals!
Understanding the Role of Estrogen and Progesterone
Estrogen plays a crucial role in the development and maintenance of breast tissue, enhancing its density and stimulating growth. Conversely, progesterone prepares the breasts for potential pregnancy, which can also lead to tenderness. Understanding how these hormonal shifts influence breast health is key to managing discomfort.
- Estrogen: Typically peaks in the first half of your cycle, promoting breast tissue growth.
- Progesterone: Rises in the second half, which can cause swelling and tenderness.
- Combined Effects: The interaction between these hormones often leads to cyclic breast pain.
By recognizing these patterns, you can better anticipate when tenderness may occur, allowing you to take proactive steps to manage discomfort!
The Biological Mechanisms Behind Breast Pain
Breast pain, or mastalgia, can be categorized into two main types: cyclic and noncyclic. Cyclic mastalgia is directly related to hormonal changes, whereas noncyclic forms may have different underlying causes. Understanding these mechanisms can empower you to differentiate between them.
- Cyclic Mastalgia: Occurs in sync with your menstrual cycle; peaks before menstruation.
- Noncyclic Mastalgia: Less predictable, often related to other factors such as stress or injury.
- Impact of Hormonal Fluctuations: Significant shifts in hormone levels can trigger breast discomfort.
By understanding these distinctions, you can better assess your symptoms and determine whether they warrant further investigation. If you experience persistent pain, I encourage you to consult with a healthcare professional for tailored advice.
Types of Breast Pain: What You Need to Know
Breast pain can be confusing, especially when trying to identify its source. In this section, we will delve deeper into the two main types of breast pain: cyclic and noncyclic mastalgia, helping you gain clarity on what your body is experiencing.
Pro Tip
To better manage breast tenderness linked to hormonal fluctuations, consider keeping a symptom journal. Documenting your cycle, along with any discomfort experienced, can help you identify patterns and triggers, empowering you to take proactive steps for relief.
Frequently Asked Questions About Hormones and Breast Pain
- What role do estrogen and progesterone play in breast tenderness?
- Estrogen, which peaks in the first half of the menstrual cycle, promotes breast tissue growth and density, leading to increased sensitivity. Progesterone, which rises in the second half, prepares the breasts for potential pregnancy, often causing swelling and tenderness. The interaction of these hormones frequently results in cyclic breast pain.
- How can I differentiate between cyclic and noncyclic breast pain?
- Cyclic breast pain (mastalgia) is directly linked to your menstrual cycle, typically peaking before menstruation and following a predictable pattern. Noncyclic breast pain is less predictable and is usually related to other factors such as stress, injury, or underlying conditions, rather than hormonal fluctuations.
- Why is tracking hormonal fluctuations important for managing breast pain?
- Tracking hormonal fluctuations helps you understand the patterns of your breast tenderness, allowing you to anticipate when discomfort may occur. This knowledge empowers you to take proactive steps to manage symptoms, such as adjusting your diet, managing stress, or seeking timely medical advice.
- What are some effective strategies to alleviate breast pain?
- Effective strategies include keeping a symptom journal to identify triggers, consulting healthcare professionals for personalized assessments, educating yourself on dietary choices that support hormonal balance, and engaging in stress-reducing activities like yoga or meditation. For persistent or severe pain, it's always best to seek professional medical advice.
- When should I be concerned about breast pain and seek medical advice?
- While most breast pain is benign and linked to hormonal changes, you should consult a healthcare professional if you experience persistent, severe, or localized pain that doesn't follow your menstrual cycle, or if you notice any new lumps, skin changes, or nipple discharge. Early consultation can help rule out more serious conditions.
Summarizing Key Findings on Hormones and Breast Pain
Throughout our exploration of breast pain, we’ve uncovered some vital connections between hormones, particularly estrogen and progesterone, and the discomfort many women experience. It's essential to recognize how these hormones fluctuate and impact breast tissue, especially during pivotal moments such as the menstrual cycle and menopause. This understanding is not just academic; it’s a pathway to better managing your breast health. For a detailed medical overview of breast pain, you can refer to resources like the National Center for Biotechnology Information (NCBI) which provides comprehensive information on mastalgia and its causes.
By acknowledging the different types of breast pain, including cyclic and noncyclic mastalgia, we can identify personalized strategies that make a real difference. Remember, knowledge is power! When you equip yourself with insights into hormonal changes and their effects, you can take proactive steps to improve your comfort and well-being. The Cleveland Clinic offers further insights into the various causes of breast pain, helping you understand when it might be related to hormonal changes versus other factors.
Empowering Readers to Take Control of Their Health
As we wrap up, I want to encourage you to be proactive about your hormonal health. It's crucial to monitor any changes in your body and understand how they relate to your hormonal fluctuations. Here are some empowering strategies to help you manage your breast pain:

- Keep a journal to track your symptoms and identify potential triggers.
- Consult with healthcare professionals for personalized assessments.
- Educate yourself on dietary choices that support hormonal balance.
- Engage in stress-reducing activities, such as yoga or meditation.
Taking the initiative in your health journey can lead to more effective symptom management. Don’t hesitate to seek support, whether through online resources, community groups, or healthcare providers! For more information on managing breast pain, including various treatment options, you might find this article from PubMed beneficial, as it discusses the efficacy of different treatments for mastalgia.
Resources for Further Reading and Support
For those who wish to delve deeper into the topic of breast pain and hormonal health, there are many reputable resources available to you. At Breast Tenderness, we strive to provide a wealth of information, but you might also find these additional resources helpful:
- American College of Obstetricians and Gynecologists
- National Breast Cancer Foundation
- Office on Women's Health
These organizations offer expert insights and valuable support for women navigating breast health concerns. I recommend checking their resources for further reading and connecting with communities that share similar experiences.
Inviting Reader Engagement and Questions
I genuinely want to hear from you! Have you experienced breast pain linked to hormonal changes? What strategies have worked for you in managing that discomfort? Please share your experiences, questions, and thoughts in the comments below. At Breast Tenderness, we aim to create a community of support where women can share their stories and insights. Your voice matters, and together, we can foster a space for learning and growth!
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Estrogen and progesterone play crucial roles in breast tissue health and tenderness, with estrogen increasing sensitivity in the first half of the menstrual cycle and progesterone causing swelling in the second half.
- Cyclic mastalgia is linked to hormonal changes during the menstrual cycle, while noncyclic mastalgia may arise from stress or injury.
- Keeping a symptom journal can help identify triggers and patterns related to breast pain, enabling better management strategies.
- Engaging in stress-reducing activities and consulting healthcare professionals are essential steps for managing breast tenderness effectively.








